Select everything that applies to you:

We recommend:
Flush
We recommend Flush because you want better urinary tract health.
Flush is a drink mix that proactively flushes the urinary tract. Ingredients help to alkalize the urine, plus binds to microorganisms in the urine and flushes them from the urinary tract.
Try risk free with our 60 day money back guarantee!

We recommend:
Defend
We recommend Defend because you said urinary tract health affects you 3+ times a year. Defend cleanses biofilm, which helps to keep the urinary tract clear on a day-to-day basis. It also supports bladder wall integrity.
(Psst, we really recommend you also try Flush (our drink mix) to flush your urinary tract in addition to Defend since you’re frequently affected by urinary tract health. Find that bundle here.)
Try risk free with our 60 day money back guarantee!
We recommend:
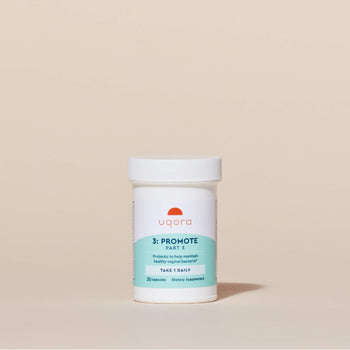
Promote
We recommend Promote because vaginal health is tightly linked to urinary tract health. Vaginal pH can be affected by a variety of ways including hormonal changes, sex, menstruation, and more. Promote supplies this “good” vaginal bacteria (lactobacillus) to support vaginal health.
(Psst, if you also struggle with urinary health issues we really recommend you also try Flush (our drink mix), which is crucial for urinary health support.)
Try risk free with our 60 day money back guarantee!

We recommend:
Flush & Defend
Flush, because you want better urinary tract health.
Flush is a drink mix that flushes the urinary tract. Drink Flush every 3 days and immediately after sex, if sexually active.
Defend, because you said urinary tract health affects you 3+ times a year. Defend supports bladder wall integrity and continually cleanses biofilm, which is key for day-to-day urinary tract health. Take two capsules a day.
Try risk free with our 30 day money back guarantee!

We recommend:
Flush & Promote
Flush, because you want better urinary tract health.
Flush is a drink mix that flushes the urinary tract. Drink Flush every 3 days and immediately after sex, if sexually active.
Promote, because sex and hormonal changes (especially menopause) affect your vaginal microbiome, and impact urinary tract health.
Promote is a probiotic for your vagina, which supplies good bacteria (lactobacillus) to keep your vagina balanced—a key component of urinary tract health. Take one capsule a day.
Try risk free with our 60 day money back guarantee!

We recommend:
Defend & Promote
Defend, because you said urinary tract health affects you 3+ times a year. Defend supports bladder wall integrity and continually cleanses biofilm, which is key for day-to-day urinary tract health. Take two capsules a day.
(Psst, we really recommend you try Flush to flush your urinary tract in addition to Defend since you’re frequently affected by urinary tract health. Find that bundle here.)
Promote, because sex and hormonal changes (especially menopause) affect your vaginal microbiome, and impact urinary tract health. Promote is a probiotic for your vagina, which supplies good bacteria (lactobacillus) to keep your vagina balanced—a key component of urinary tract health. Take one capsule a day.
Try risk free with our 60 day money back guarantee!

We recommend:
Complete Regimen
We recommend our Complete Regimen — 3 products intentionally designed to provide our maximum support.
✔️Flush is a drink mix that proactively flushes the urinary tract.
✔️Defend cleanses biofilm and supports bladder wall integrity, which is key for day-to-day urinary tract health.
✔️Promote is a probiotic for your vagina, that supplies good vaginal bacteria (lactobacillus). Vaginal health is a key component of urinary tract health.
Each product has a distinct function and supports you in a different way, keeping you covered from multiple angles.
Try risk free with our 60 day money back guarantee!






















